By Ada Jane Okonkwo (BCANDS)

Disability and Indigenous communities
As we acknowledged Indigenous Disability Awareness Month this past November, it was especially important to recognize the impact of the COVID-19 pandemic on Indigenous persons with disabilities and their families in Canada. Indigenous Peoples of Canada represent 4.9% of the total population (roughly 1.7-million). However, when comparing rates of disability, the rate of Indigenous persons with disabilities is estimated to be between 30-35%, compared with 22% among non-Indigenous communities. The rate of disability in Indigenous communities may be higher still. A recent report released by Statistics Canada estimates that one in three First Nations people living off-reserve and Métis have a disability and one in five Inuit have a disability (Hahmann, Badets, Hughes, 2019).
Historically, Indigenous Peoples of Canada have suffered from devastating viruses introduced by colonial settlers. Waves of epidemics of smallpox, tuberculosis, scarlet fever, influenza and measles wiped out communities and had long-lasting impacts. While COVID-19 has impacted the lives of all Canadians, the nature of Indigenous Peoples’ complex barriers and existing underlying health conditions and challenges means they are at a greater risk of suffering long-term complications from contracting the virus.
COVID-19 and its impact
The COVID-19 global pandemic has amplified existing social and health inequities and barriers for many Indigenous communities including access to culturally appropriate health care services and testing, direct home support, transportation, culturally safe programming, adequate living conditions, employment, healthy food, mental health support, technology, and internet services to connect virtually. For Indigenous persons with disabilities and their families, living in isolated or remote communities amplifies these barriers further.
History has also strengthened the resilience of Indigenous communities to effectively plan, manage and monitor pandemics and diseases. To better understand the needs and priorities of Indigenous persons with disabilities and their families across Canada, the British Columbia Aboriginal Network on Disability Society (BCANDS) launched a COVID-19 Indigenous Engagement Program. This program involves an online survey, focus groups and one-on-one interview sessions. This program also aims to gather innovative and sustainable solutions to meet the needs of Indigenous persons with disabilities and their families during COVID-19 and beyond.
During the first wave in August, fewer than 467 COVID-19 cases in First Nations communities were reported by Indigenous Services Canada (ISC). The second wave is surging and impacting Indigenous communities with disabilities even harder. As of November 26, 2020, ISC reported:
- 3,451 confirmed positive COVID-19
- 1,400 active cases
- 152 hospitalizations
- 2,022 recovered cases
- 29 deaths
Case numbers per region:
- British Columbia: 228
- Alberta: 1,093
- Saskatchewan: 939
- Manitoba: 861
- Ontario: 185
- Quebec: 145
Although this data provides context to the situation in First Nations communities, it fails to capture the true number of COVID-19 cases for Indigenous persons living in urban communities, and Métis and Inuit communities.
Has the government’s response been enough?
Since the start of the pandemic, the Government of Canada has partnered with First Nations, Inuit and Métis organizations to support Indigenous communities to prepare for, monitor and respond to COVID-19. However, these supports have not been sufficient in meeting the needs of Indigenous persons with disabilities and their families. Most importantly, disaggregated data is not available, therefore limiting COVID-19 resources and supports that are distributed to Indigenous communities. Service providers and community members across Canada suggest an existing lack of adequate resources to meet the needs of Indigenous persons with disabilities in their community. Here are some quotes from family members and services providers to Indigenous persons with disabilities across Canada that highlight the reasons many of the current COVID-19 supports have not been sufficient:
“There is no transportation and inadequate housing for PWD up North”~ Ona
“Now more than ever, we need increased outreach, virtual connections/community, virtual support groups and Elder to youth peer connections to maintain culture, and transfer knowledge” – Rheanna
“Individuals living with disabilities have increased isolation as a result of COVID-19. They have been left to isolate and without any access to the internet, they are experiencing further isolation. Unable to attend religious services and support groups for community members who found social connections through this method. This has been a huge barrier for PWD during the pandemic” compared to the general population…” it is worth continuing the conversation beyond zoom, we are concerned for the short term needs of winter preparedness. If folks had limited access to basic necessities in the summer, imagine how they can manage services during the winter. Mental wellness will be impacted during the winter months- a Northern BC community
“Since cultural activities and gatherings have been stopped or moved virtually, this is still limited because people are unable to come together and connect in person. Inequalities and issues that existed before COVID-19 has now worsened since the pandemic. Housing, racism, and discrimination have worsened. Long term, we need emotional support, which may not include things like Zoom, we need support systems that are modified to accommodate the mental and support needs of persons with disabilities” – a Friendship centre
“Food insecurity continues to impact our communities, clients with disabilities are unable to prepare their own food especially with support workers not able to come into their homes to help them cook the meals, so the food that they receive they are unable to eat” had to get creative with meal drop-offs and hot food delivery. The funding has been inconsistent and unsure of whether the funding will be sustained. Difficulties preparing food with a PWD”. – a Friendship Centre
“We need more financial help for our elders, OAS is not enough for them to survive. Everyone else is getting financial help why not Elders?”. – a First Nation community
Using traditional knowledge as a solution to manage COVID-19
Empowered by the long-lived experience and teachings on previous pandemics that were gathered from knowledge keepers, Indigenous communities are using traditional knowledge to seek their own solutions to manage, plan, and prepare for potential COVID-19 outbreaks. To keep the most vulnerable members in their communities safe – Elders and persons with disabilities, Indigenous communities are adapting and “providing culturally appropriate supports, such as virtual pow-wows, and singing specials online” ~ Gina.
We are seeing these innovative solutions emerge across the country. With respectful partnership and intentional collaboration, Indigenous communities are coming together to provide innovative Indigenous health solutions that centre the cultural, spiritual and holistic well-being of its people and in a way that is free from racism. BCANDS is an example of an Indigenous-led organization that continues to centre the disability and health needs of Indigenous persons.
In the first wave of the COVID-19 pandemic, BCANDS conducted virtual wellness checks to its most vulnerable members. These wellness checks reduced isolation and encouraged positive interactions for our community. In anticipation of the pandemic’s second wave, BCANDS launched an Indigenous Support for Student Learning Program (SSLP) to provide laptops to low-income Indigenous students across Canada. This program enables the continued education and success for Indigenous students of any age who are enrolled in formal education. This program is crucial in these times when isolation is high, mental wellness is low, and access to the virtual world is required for education and otherwise.
Another example of an ongoing collaboration to sustain Indigenous health and well-being and that we can all learn from is the Indigenous-led COVID-19 testing centre in Toronto at Na-Me-Res.
In one remote community where airplanes are the main transportation, health directors have set plans to ensure that the needs of vulnerable persons, such as Elders and PWD, is a priority. Members of the community who leave for medical appointments and rehabilitation are required to isolate for 14 days and most importantly, contacts of members entering and exiting the community are in place and permit adequate contact tracing for any potential outbreaks. Persons suffering from additions are supported and monitored throughout their rehabilitation process. Persons with disabilities are offered grocery support, home visits, and the cars used by community health representatives are equipped with lifts to accommodate PWD. Most notably, these plans were set in place and led by Indigenous peoples.
Throughout this COVID-19 Indigenous community-led engagement processes initiated by BCANDS, innovative supports and solutions that may benefit the longevity, well-being and health outcomes of Indigenous peoples during COVID-19 and beyond are highlighted. To ensure the needs and priorities of Indigenous persons with disabilities and their families are met, we need to continue to advocate and work alongside Indigenous communities to develop culturally appropriate ways to create awareness of Indigenous persons with disabilities and their families.
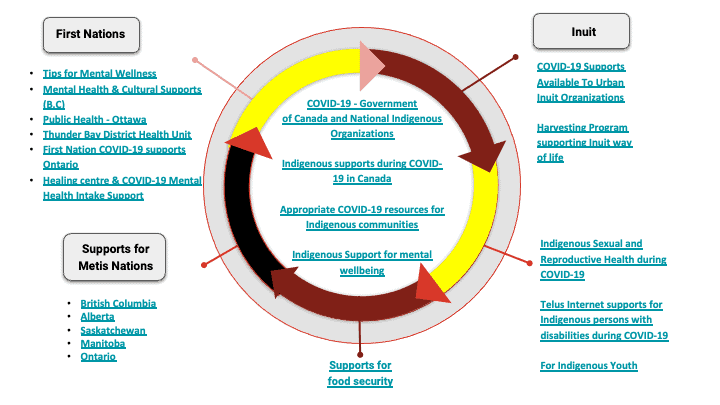
For more information on mental wellness supports, food resources, and ideas on how to reduce isolation, please click on the accessible infographic below:
COVID-19 Resource Accessible Indigenous Infographic
The COVID-19 Indigenous Engagement Program is expected to last until March 31, 2021. This program seeks to identify the barriers, provide resources and support to Indigenous persons with disabilities and their families during COVID-19.
BCANDS continues to engage members of First Nations, Métis, and Inuit communities across Canada, by collecting data through surveys, focus groups and one-on-one interviews. The data collected from your communities during this research will inform the recommendations made to back to your community, the Convention on the Rights of Persons with Disabilities (CRPD), government officials, and Indigenous policy-makers.
To participate in the survey: https://www.surveymonkey.com/r/ImpactofCOVID-19onIndigenousPeoplesLivingwithaDisability
For more information:
Contact BCANDS’ COVID-19 Coordinator-
Toll-Free: 1-888-815-5511 ext. 217
Capital Region: (250) 381-7303 ext. 217
Email: covidlead@bcands.bc.ca
Twitter: @IndigenousCOVID
 Ada Jane Okonkwo is the COVID-19 Indigenous Engagement Coordinator for the BC Aboriginal Network on Disability Society. Ada acknowledges and respectfully thanks the Lekwungen-speaking peoples, also known as the Songhees and Esquimalt First Nations communities, for allowing us to live, work and play on their lands. She graduated from the Interdisciplinary Health Sciences program at the University of Manitoba, and since then has over 6 years of working as a community coordinator prior to working with BCANDS.
Ada Jane Okonkwo is the COVID-19 Indigenous Engagement Coordinator for the BC Aboriginal Network on Disability Society. Ada acknowledges and respectfully thanks the Lekwungen-speaking peoples, also known as the Songhees and Esquimalt First Nations communities, for allowing us to live, work and play on their lands. She graduated from the Interdisciplinary Health Sciences program at the University of Manitoba, and since then has over 6 years of working as a community coordinator prior to working with BCANDS.
**Please note that all views and opinions expressed by contributors should be recognized as theirs alone, and do not necessarily reflect the official policies or position of Plan Institute**